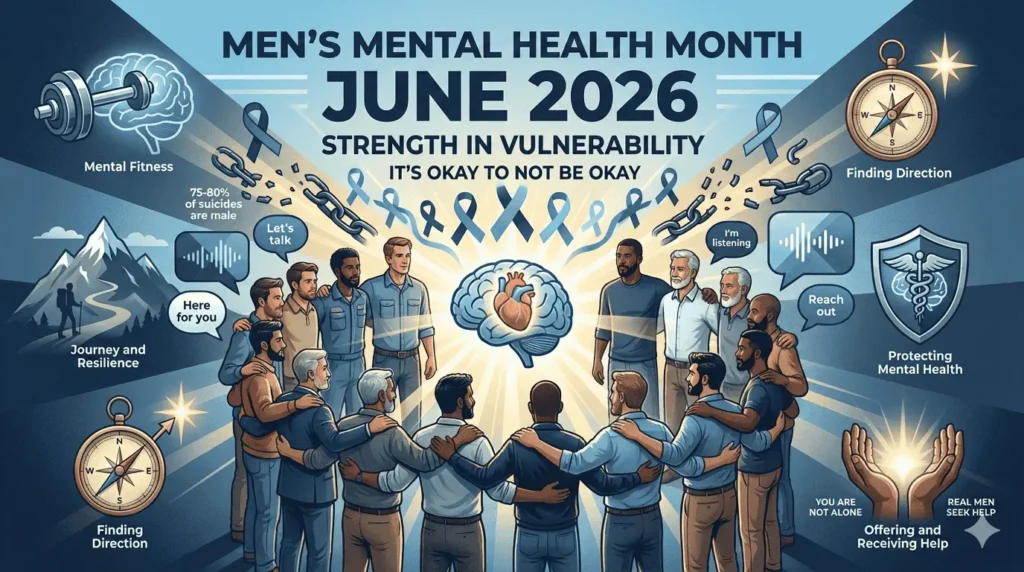
Men's mental health month saves lives. Every June, we shine a spotlight on male mental wellness—a topic that's too often overlooked. Men face unique mental health challenges. They're less likely to seek help. They die by suicide at alarming rates. This comprehensive guide covers everything you need to know about men's mental health month. You'll learn when it's observed, why it matters, and how to support the men in your life. Whether you're a man struggling with mental health, a loved one wanting to help, or an advocate working to break stigma, this resource is for you. Men's mental health awareness month creates conversations that save lives. Let's start talking.
Understanding Men's Mental Health Awareness Month
When Is Men's Mental Health Month Observed?
Men's Mental Health Month happens every June. What month is men's mental health month? June. This annual observance dedicates an entire month to male mental wellness. June men's mental health month addresses the specific needs and challenges men face. The observance has gained growing recognition since the early 2000s. It's now a national observance in the United States, with international attention expanding each year.
What Month Is Men's Mental Health Month and Why June?
Why June? The timing connects powerfully with Father's Day, celebrated on the third Sunday in June. This highlights paternal mental health and the pressures fathers face. Summer timing allows for outdoor awareness events and community gatherings. It falls during academic year transitions, making it ideal for youth mental health initiatives. June also overlaps with Pride Month, bringing attention to LGBTQ+ male mental health. The midpoint timing between other mental health awareness efforts keeps the conversation going year-round.
History of Men's Mental Health Awareness Month
Men's mental health awareness month emerged as a response to alarming male suicide statistics. Advocates recognized that men were dying silently, reluctant to seek help. The observance addresses masculinity and mental health stigma head-on. It complements Movember, the November men's health initiative that includes mental health focus. What started as grassroots advocacy has grown into a recognized observance. Mental health organizations, corporations, and media outlets now participate annually. The awareness continues expanding each year.
Related Men's Health Observances
Several other dates focus on men's health throughout the year. Movember (November) emphasizes men's health awareness with a strong mental health component. International Men's Day (November 19) celebrates global male wellness. Men's Health Week, the week before Father's Day, addresses both physical and mental health. World Suicide Prevention Day (September 10) highlights male suicide prevention efforts. These observances work together to keep men's mental wellness in the conversation.
The Critical Need for Men's Mental Health Awareness
Alarming Statistics
The numbers tell a devastating story. Men die by suicide at three to four times the rate of women. Seventy-five to eighty percent of suicide deaths are male. Men are 40% less likely to seek mental health treatment than women. Only one in three men talk about their mental health concerns. Depression in men often goes undiagnosed because symptoms present differently. Substance abuse rates are higher in males. Male veterans face elevated PTSD risks. Men ages 45-64 represent the highest suicide risk group. These aren't just statistics. They're fathers, brothers, sons, and friends we're losing.
Unique Challenges Men Face
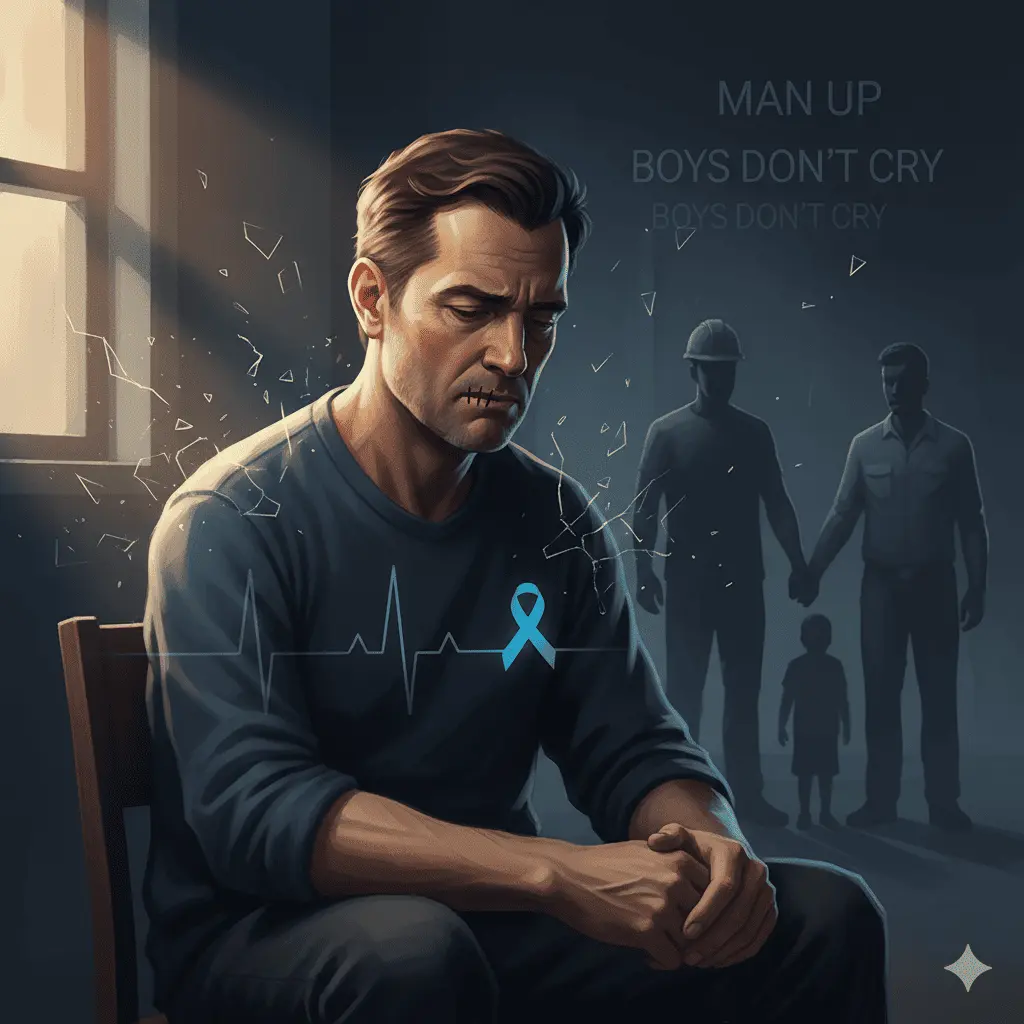
Men face specific barriers to mental wellness. Cultural masculinity norms start in childhood. "Man up" messaging conditions boys early. Emotional expression gets labeled as weakness. Society expects men to be providers, to be independent, to handle everything alone. Vulnerability gets stigmatized. "Boys don't cry" becomes a life sentence. Strength becomes equated with stoicism, creating dangerous silence.
Social isolation compounds the problem. Men typically have smaller support networks than women. Male friendships, while valuable, are often less emotionally intimate. There's reluctance to reach out for help. Workplace competition creates barriers to vulnerability. Post-retirement, social disconnection intensifies. Many men never develop the emotional vocabulary they need.
Men express depression differently than women. Anger and irritability appear more common than obvious sadness. Risk-taking behaviors increase. Substance use becomes self-medication. Physical symptoms get emphasized over emotional ones. This "masked depression" in males means traditional screening often misses the signs.
The Silence That Kills
Why don't men seek help? Fear of appearing weak tops the list. Stigma runs especially deep in male-dominated workplaces. There's a lack of mental health literacy among men. Healthcare system navigation feels challenging. Financial concerns and insurance barriers exist. Many men don't recognize their symptoms as mental health issues. Previous negative experiences with help-seeking create avoidance. The belief that "real men" should handle problems alone runs deep.
This silence has devastating impacts. Delayed treatment worsens outcomes. Relationships suffer and deteriorate. Physical health declines. Work performance drops. Substance abuse escalates. Suicide risk increases dramatically. The cost of silence is measured in lives lost.
Mental Health Conditions in Men
Depression in Men
Male depression looks different. Anger, irritability, and aggression appear more prominently than sadness. Escapist behaviors increase—working excessively, engaging in sports obsessively, or hypersexual behavior. Risky activities and reckless driving become more common. Alcohol and drug abuse mask underlying pain. Physical complaints like headaches and digestive issues dominate. Sleep disturbances, fatigue, low energy, and difficulty concentrating all appear. Loss of interest in activities once enjoyed signals trouble.
Traditional depression screening misses male symptoms. Men minimize emotional distress. They get labeled as "stressed" rather than depressed. Self-medication masks the underlying condition. Recognition remains a critical challenge.
Anxiety Disorders in Men
Male anxiety often manifests as physical symptoms. Chest pain and heart palpitations create fear. Muscle tension and headaches become chronic. Digestive problems develop. Restlessness and agitation appear constant. Work-related stress and worry consume mental energy. Social anxiety in male-dominated environments creates pressure. Performance anxiety—at work, in relationships, sexually—becomes debilitating.
Substance Use Disorders
Men show higher rates of alcohol abuse and drug addiction. Often, these link directly to untreated mental health conditions. Self-medication for depression and anxiety drives substance use. Workplace stress correlates with increased drinking. Societal acceptance of male drinking normalizes excessive use. Men find it harder to admit addiction problems, fearing judgment and weakness.
Post-Traumatic Stress Disorder (PTSD)
Male PTSD has specific risk factors. Combat veterans are disproportionately affected. First responders—firefighters, police officers, EMTs—face repeated trauma exposure. Workplace trauma, childhood abuse, and domestic violence (often silent in male victims) all contribute. Emotional numbing becomes common. Aggression and anger responses replace other emotions. Avoidance behaviors intensify.
Suicide Risk in Men
Critical warning signs demand attention. Talking about being a burden to others. Increased substance use. Acting reckless or agitated. Withdrawing from family and friends. Mood changes, especially sudden improvement after deep depression. Giving away possessions. Saying goodbye to people. Researching suicide methods. Previous suicide attempts dramatically increase risk.
Men complete suicide more often because they use more lethal methods. They're less likely to communicate intent beforehand. They act more impulsively. They have smaller support networks. They don't seek help before reaching crisis. Understanding these patterns can save lives.
Dismantling Toxic Masculinity and Mental Health Stigma
Understanding Masculinity's Impact
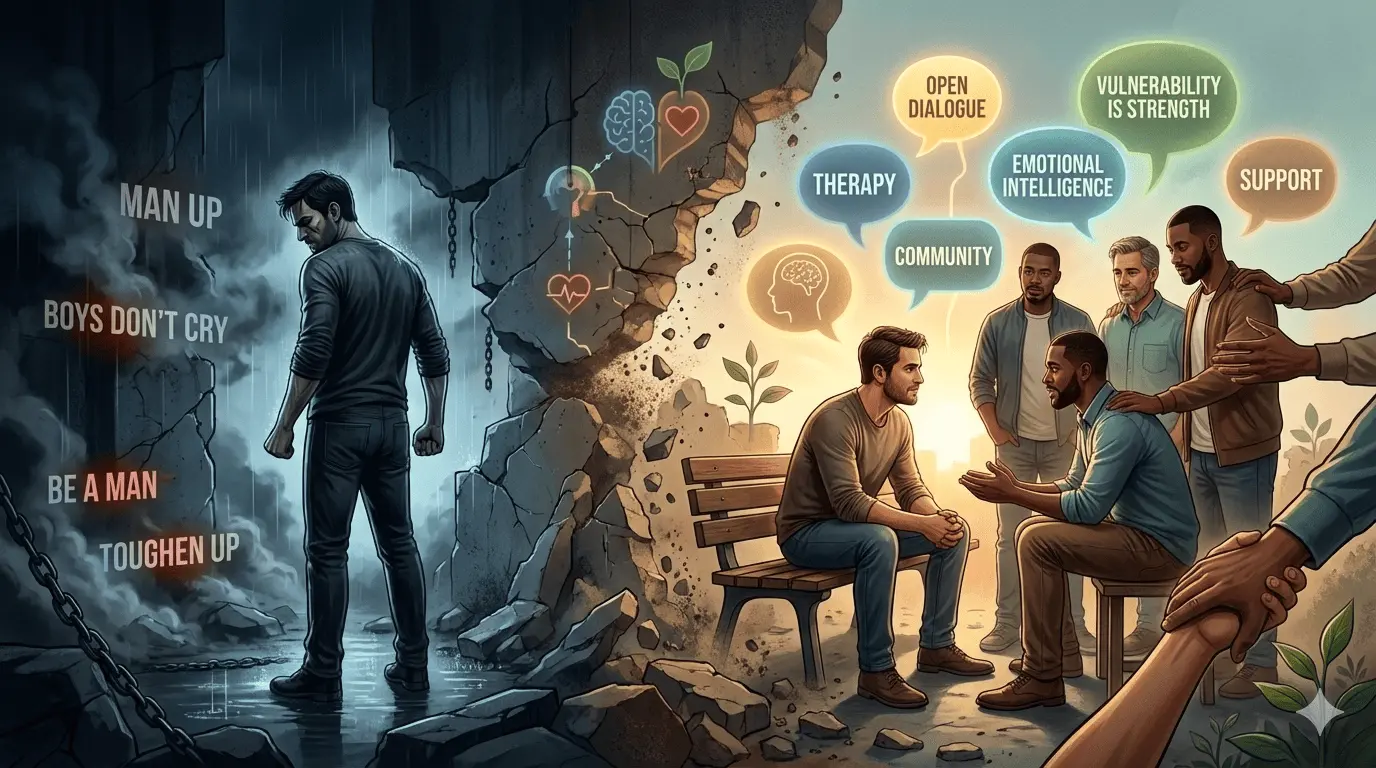
Traditional masculine norms harm mental health. Self-reliance at all costs prevents help-seeking. Emotional restriction and control create internal pressure. Dominance and aggression get valued over vulnerability. Men avoid anything perceived as "feminine," including emotional expression. Success gets defined narrowly by achievement and power. Provider and protector roles create impossible standards. Physical toughness gets emphasized. Competition wins over collaboration.
These norms prevent help-seeking behaviors. They isolate men from support. They create shame around vulnerability. They increase risk-taking and aggression. They limit emotional expression and processing. They damage relationships and intimacy. They contribute to substance abuse. They elevate suicide risk significantly.
Redefining Strength
Healthy masculinity embraces different concepts. Strength includes asking for help. Vulnerability is courage, not weakness. Emotional intelligence demonstrates power. Connection and community matter deeply. Self-care is masculine. Mental fitness equals physical fitness. Expressing feelings promotes health. Seeking therapy shows wisdom and self-awareness.
Language That Helps vs. Harms
Words matter. Harmful phrases include "man up," "be a man," "boys don't cry," "don't be a pussy," "toughen up," "stop being emotional," and "real men don't need therapy." These phrases kill.
Supportive alternatives save lives. "It's okay to struggle." "Asking for help is brave." "Your feelings are valid." "I'm here if you want to talk." "Taking care of mental health is important." "Many men experience this." "Therapy is a tool, like going to the gym." These phrases open doors.
Creating Male-Friendly Mental Health Culture
Workplaces can implement male mental health champions, men's peer support groups, and mental health training for managers. Normalize therapy and counseling. Offer flexible work for mental health days. Create open dialogue about stress. Have leadership model vulnerability.
Communities can organize men's mental health events, sports-based mental health programs, and barbershop mental health conversations. Establish male-focused support groups and peer-to-peer networks. Create online communities for men. Develop father-specific mental health resources.
Supporting Men's Mental Health Awareness in June
Individual Actions for Men
If you're struggling, start by recognizing and acknowledging your symptoms honestly. Acknowledge that mental health is health. Understand that seeking help demonstrates strength. Your struggle doesn't define your manhood. Many successful men face mental health challenges. Treatment works effectively.
Take the first step. Talk to someone you trust. Schedule a doctor or therapist appointment. Call the 988 Suicide & Crisis Lifeline. Try online therapy if in-person feels difficult. Join a men's support group. Download a mental health app. Start with anonymous online resources if you need to.
Build your support network. Open up to one trusted friend. Join men-specific mental health communities. Connect with other fathers if applicable. Find a male mentor who values mental health. Engage in group activities like sports or hobbies. Explore online forums for men's mental health.
How to Support Men in Your Life
Check in meaningfully. Ask "How are you really doing?" Create judgment-free space. Don't dismiss or minimize concerns. Avoid jumping into "fix-it" mode—just listen. Make regular check-ins, not just crisis interventions. Notice behavior changes. Express concern without judgment.
Encourage help-seeking. Normalize therapy and counseling. Offer to help find resources. Attend appointments if wanted. Frame mental health care as health maintenance. Share stories of men who sought help successfully. Emphasize strength in vulnerability. Be patient with resistance.
Provide practical support. Help with daily tasks during hard times. Reduce household stress when possible. Encourage healthy habits. Engage in activities together. Respect the need for space when requested. Stay connected consistently.
Workplace and Community Activities
Office initiatives during men's mental health month can include lunch and learns, sharing male mental health statistics, inviting male speakers in recovery, distributing men's resources, forming men's support groups, promoting mental health day policies, and training managers on male mental health.
Community events might include men's mental health walks or runs, barbershop talk events, sports-based awareness activities, Father's Day mental health focus, panel discussions with male speakers, screening and resource fairs, and men's wellness workshops.
Schools and youth programs should talk to boys about emotional health, provide male role models discussing mental health, incorporate mental wellness into sports programs, organize father-son mental health activities, establish teen boys support groups, and teach healthy masculinity.
Social Media Advocacy
Use social media to share men's mental health statistics and resources. Use hashtags like #MensMentalHealthMonth, #JuneMentalHealth, and #ItsOkayToTalk. Post resources specifically for men. Share personal stories if comfortable. Amplify male mental health advocates. Challenge toxic masculinity posts. Support men sharing vulnerably. Promote the 988 hotline widely.
Create visual campaigns using blue ribbons for men's health awareness, profile pictures highlighting the cause, infographics about male suicide rates, and quotes from men about seeking help successfully.
Mental Health Support Specifically for Men
Crisis Support for Men (24/7 Help)
If you're in crisis right now, help is available immediately.
988 Suicide & Crisis Lifeline: Call or text 988. Available 24/7. Free and confidential. Trained crisis counselors understand what you're going through.
Crisis Text Line: Text HOME to 741741. Available 24/7. Anonymous and confidential. Text-based support for men who prefer not to talk on the phone.
Veterans Crisis Line: Call 988 and press 1. Text 838255. Chat at VeteransCrisisLine.net. Veteran-specific support for male veterans.
Man Therapy: Visit mantherapy.org. Male-focused mental health resource with a humorous, accessible approach. Includes screening tools and resources.
Men's Mental Health Organizations
Movember Foundation (movember.com): Men's health awareness with mental health focus, resources, campaigns, community fundraising, and research funding.
Men's Health Network (menshealthnetwork.org): Mental and physical health resources, screening information, and educational materials.
HeadsUpGuys (headsupguys.org): Depression resources specifically for men, self-check tools, and anonymous support.
Postpartum Support International (postpartum.net): Paternal postpartum depression resources, father-specific support, and peer connections.
Man Therapy (mantherapy.org): Engaging male-friendly content, depression and anxiety resources, and suicide prevention tools.
Therapy Options for Men
Consider therapists specializing in men's issues. Male therapists if you prefer. Online therapy for privacy (BetterHelp, Talkspace). Group therapy specifically for men. Sports psychology approaches. Walk-and-talk therapy. Short-term solution-focused therapy.
Find the right fit by asking about experience with male clients. Discuss communication preferences. Try several therapists if needed. Consider a male therapist if more comfortable. Explore online options to reduce barriers. Check if they address masculinity issues specifically.
Support Groups for Men
Peer support options include local men's mental health groups, NAMI men's support groups, father support groups, veterans support groups, men's grief support, divorce support for men, addiction recovery groups (AA, NA), and online men's mental health forums.
Addressing Diverse Men's Mental Health Needs
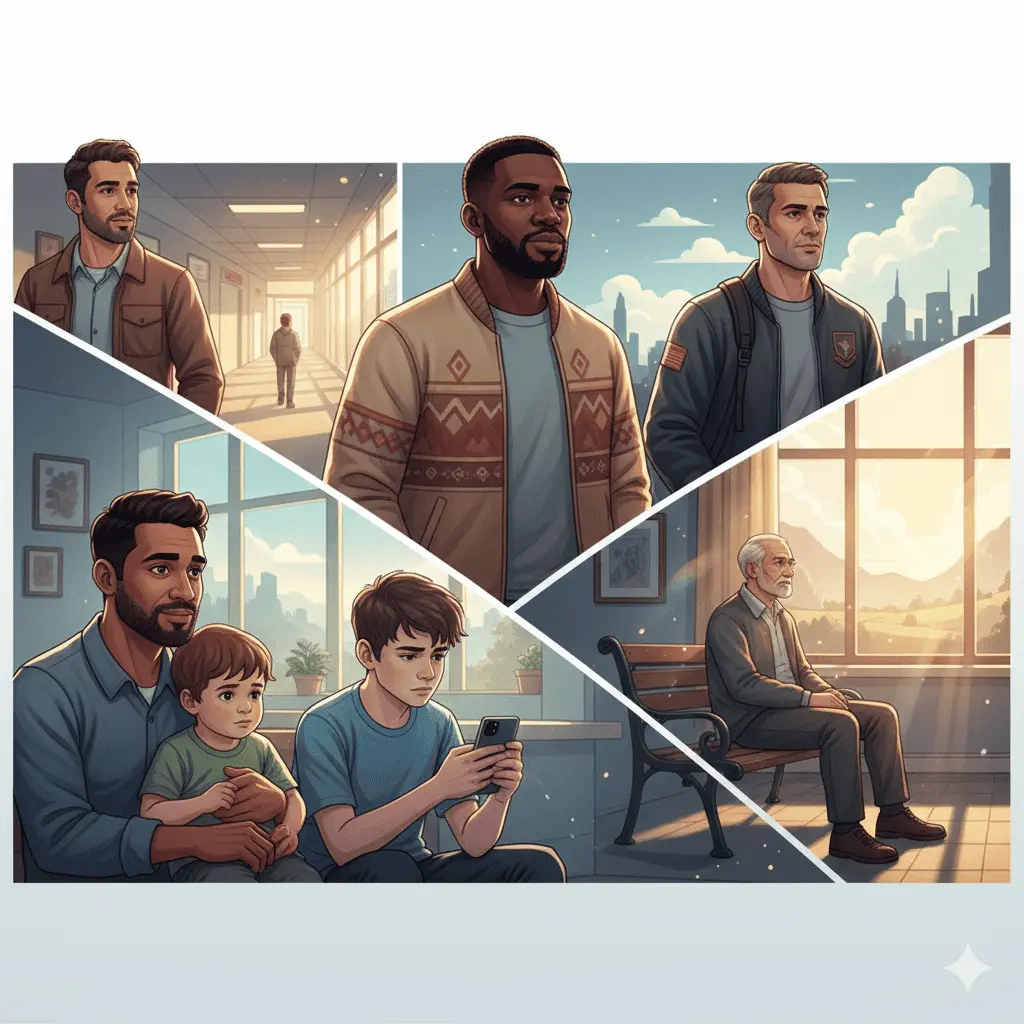
Fathers and Paternal Mental Health
Fathers face specific challenges. Paternal postpartum depression affects 10% of fathers. Provider role pressure intensifies. Work-life balance creates stress. Identity changes with fatherhood. Single fathers face unique stressors. Custody and co-parenting create stress. Fear of appearing inadequate prevents help-seeking. Limited father-focused resources exist.
Support fathers by normalizing paternal mental health struggles, creating father-specific support groups, involving partners in mental health, providing workplace paternity leave support, and having Father's Day mental health conversations.
Young Men and Boys
Teen male suicide rates are rising. Social media creates pressure and comparison. Academic performance stress increases. Masculinity confusion occurs during development. Bullying and peer pressure intensify. Athletic performance pressure mounts. Early intervention is critical.
Support young males by teaching emotional vocabulary early, modeling healthy emotional expression, creating safe spaces for vulnerability, challenging "boys will be boys" mentality, ensuring school counseling access, establishing peer support programs, and providing male role models who discuss feelings openly.
Men of Color
Men of color face compounded stigma from both race and gender. Cultural masculinity norms vary. Historical medical mistrust creates barriers. Access to care remains limited. Discrimination stress accumulates. Cultural expressions of distress differ. Culturally competent care is essential.
Black men face higher trauma exposure, police violence stress, economic stressors, and the "strong Black man" stereotype. Community-based support proves especially important.
Latino men navigate machismo cultural factors, immigration-related stress, family pressure and expectations, language barriers to treatment, and need cultural therapy approaches.
LGBTQ+ Men
LGBTQ+ men experience unique stressors including minority stress, coming out challenges, discrimination and rejection, and family acceptance issues. They face higher rates of depression and anxiety and elevated suicide risk. Gender expression and masculinity intersect complexly. Finding affirming care is essential.
Older Men and Seniors
Aging men face retirement identity loss, increasing social isolation, widowhood and grief, physical health decline stress, purpose and meaning challenges, and "successful aging" pressure. This often-overlooked population needs targeted support.
Veterans and First Responders
Veterans and first responders face higher PTSD prevalence, traumatic exposure, hypermasculine work cultures, difficult transitions (military to civilian), moral injury, occupational stigma against seeking help, and need specialized treatment approaches.
Building Mental Wellness: Self-Care for Men
Reframing Self-Care as Masculine
Self-care isn't selfish. Mental fitness equals physical fitness. Maintenance prevents breakdown. You're stronger for others when you're healthy. Champions train and recover. Taking care of yourself is responsible. Self-care improves performance. Leaders prioritize their wellness.
Practical Mental Health Strategies for Men
Physical wellness includes exercise as a mental health tool, team sports for connection, weightlifting for stress relief, outdoor activities in nature, sleep hygiene (7-9 hours), nutrition supporting mental health, and limiting alcohol and substances.
Emotional management involves developing emotional vocabulary, journaling or voice recording thoughts, practicing identifying feelings, expressing emotions constructively, anger management techniques, stress reduction practices, and mindfulness or meditation (reframe as "mental training").
Social connection means maintaining male friendships, joining interest-based groups, participating in men's groups or support circles, volunteering and helping others, spending quality time with partner and family, reaching out when struggling, and being vulnerable with trusted friends.
Purpose and meaning encompasses engaging in meaningful work, pursuing hobbies and passions, taking mentorship roles, community involvement, goal-setting and achievement, continuous learning, and legacy building.
When to Seek Professional Help
Seek support when symptoms persist beyond two weeks, daily functioning becomes impaired, thoughts of self-harm or suicide appear, substance use increases, relationship problems escalate, work performance suffers, physical health declines, or anger outbursts increase.
Take action by scheduling a doctor appointment, asking for mental health screening, requesting a therapy referral, trying online therapy first if hesitant, calling 988 if in crisis, joining a support group, or opening up to a trusted person.
Year-Round Men's Mental Health Advocacy
Sustaining Awareness After June
Men's mental health matters every day, not just during men's mental health awareness month. Check in on male friends regularly. Continue normalizing vulnerability. Challenge toxic masculinity year-round. Support men seeking help always. Stay educated on men's issues. Advocate for male-friendly resources. Keep the conversation going.
Creating Lasting Change
Cultural shifts needed include media representation of male vulnerability, healthcare systems addressing male needs, workplace policies supporting men, educational systems teaching emotional health, community resources for men, father-focused mental health support, and male mental health research funding.
Policy and Advocacy
Systemic changes include mental health parity enforcement, insurance coverage for men's therapy, workplace mental health programs, school mental health education, suicide prevention funding, veterans mental health services, crisis intervention training, and male-specific mental health research.
Being an Ally to Men's Mental Health
Everyone has a role. Listen without judgment. Encourage men to seek help. Challenge harmful masculine norms. Model healthy emotional expression. Support men in your life actively. Share resources proactively. Vote for mental health funding. Normalize men's therapy and counseling consistently.
Recovery and Hope for Men's Mental Health
Treatment Works
Evidence-based approaches prove effective. Therapy works highly effectively for men. Medication helps many males. Combination treatment often provides optimal results. Male-specific interventions exist and succeed. Recovery is possible and common. Relapse doesn't mean failure—it's part of the journey. Support groups work effectively for men.
Men Who Speak Out
Celebrity advocates help normalize male mental health. Dwayne "The Rock" Johnson speaks about depression. Ryan Reynolds discusses anxiety openly. Michael Phelps shares his struggles with depression and suicidal thoughts. Prince Harry advocates for therapy and mental health. Kid Cudi talks about depression and suicidal thoughts. Terry Crews champions emotional vulnerability. Common discusses therapy and healing.
These stories matter because they normalize male mental health struggles, show that successful men seek help, reduce stigma through visibility, demonstrate strength in vulnerability, encourage other men to open up, and prove mental health doesn't limit success.
Creating Your Own Recovery Story
Your journey starts where you are. Progress isn't linear—there will be setbacks. Seek help when needed without shame. Build your support system intentionally. Practice self-compassion consistently. Celebrate small wins along the way. Remember: your story can help others.
Men's Mental Health Month Starts a Lifelong Conversation
Men's mental health month happens every June. But the conversation must continue year-round. Men's mental health deserves attention, resources, and action. Seeking help is strength, not weakness. You don't have to handle everything alone. Recovery is possible. Treatment works. You matter.
This June men's mental health month, check in on the men in your life. A simple conversation can save a life. If you're struggling right now, reach out today. Call or text 988. Text HOME to 741741. You're not alone in this. Help is available right now.
Share this guide with men you care about. Together we can break the stigma around men's mental health. What will you do this men's mental health awareness month? Start the conversation today. Lives depend on it.
Frequently Asked Questions About Men's Mental Health Month
Q: When is Men's Mental Health Month?
Men's Mental Health Month is observed every June. June men's mental health month is dedicated annually to raising awareness about male mental wellness, addressing unique challenges men face, reducing stigma around help-seeking, and encouraging men to prioritize their mental health.
Q: Why do men need a dedicated mental health awareness month?
Men die by suicide at three to four times the rate of women, yet they're 40% less likely to seek mental health treatment. Men's mental health awareness month addresses masculinity stigma, encourages help-seeking, and highlights that mental wellness is masculine strength, not weakness.
Q: What are the signs of depression in men?
Male depression often appears as anger, irritability, and aggression rather than sadness. Men may display escapist behaviors, increased substance use, risk-taking, physical complaints, sleep disturbances, and loss of interest in activities. These symptoms differ from typical depression presentations, causing missed diagnoses.
Q: How can I support a man struggling with mental health?
Ask "How are you really doing?" without judgment. Listen without trying to fix. Normalize therapy as strength. Help find resources. Check in regularly, not just during crisis. Respect his need for space while staying connected. Encourage professional help when needed. Your support matters.
Q: Where can men get immediate mental health help?
Call or text 988 for the Suicide & Crisis Lifeline (24/7, free, confidential). Text HOME to 741741 for Crisis Text Line. Veterans call 988 and press 1. Visit mantherapy.org for male-focused resources. Online therapy platforms offer private support. Help is available now.